

Were deemed to have met the Medicare Conditions of Participation The legislation gave it “deemed” status, meaning that hospitals that were accredited by JCAH

The enactment of Medicare in 1965 was a watershed moment for JCAH , who consistently claimed this to be the prerogative of physicians. An early effort to include evaluation of clinical care was shot down by the AMA Surveys focused only on the hospital environment, what Donabedian would later call “structure.” They examined physical aspects, such as proper use of autoclaves, function of clinical laboratories, medical staff organization, and patient records. Worked out their differences and in 1951 founded the Joint Commission on Accreditation of Hospitals (JCAH) After months of wrangling, the three parties, along with the American College of Physicians (ACP), Program for internships and residencies and disliked the idea of a program run by administrators, not doctors. Got wind of this and made a counteroffer. Was interested and willing to provide financial support. It approached the American Hospital Association (AHA) Was in financial trouble and unable to sustain the program. In its initial foray surveying hospitals of 100 beds or more, only 89 of 692 hospitals surveyed met the minimum standards! Although that number was reported out to the college, the list of the names of the hospitals was burned to keep it from being obtained by the press! The hospital standards approval process was here to stay, however, and by 1950, half of all hospitals, 3290, were on the ACS Of hospital equipment and hospital work.” Ernest Codman was tapped to chair a Hospitalization Standardization Their other concern was about the lamentable state of hospitals, which led them to call for “a system of standardization The purpose was to distinguish those who were trained in surgery from others, to establish the specialty. Martin, and several others founded the American College of Surgeons (ACS) Along the way, however, he went out of his way to publicly accuse surgeons and hospitals of being more interested in making money, for which he was widely ostracized.Īt about the same time, in 1912, a prominent Chicago surgeon, Franklin H He kept meticulous records and later published his results in A Study in Hospital Efficiency. That he found it necessary to leave and found his own hospital in 1911. The Idea was sufficiently unpopular with his colleagues at the MGH
Idea, a system for following up patients after surgery to determine their outcomes. Over a short period, hospitals move from “pest houses” to essential resources and proliferated. Its roots go back to the early years of the twentieth century when medicine was undergoing rapid changes as the result of scientific advances in understanding the causes of diseases, the use of antisepsis, and the development of x-rays.
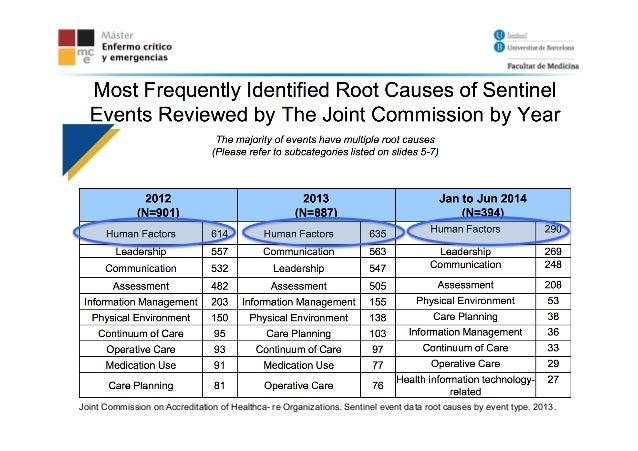
#Joint commission falls sentinel event driver
Has been for many years the principal driver of healthcare quality in hospitals and, in more recent decades, other types of healthcare organizations. Most of what follows of the early history of The Joint Commission comes from its excellent 50-year anniversary report, Champions of Quality in Health Care.


 0 kommentar(er)
0 kommentar(er)
